This topic takes on average 55 minutes to read.
There are a number of interactive features in this resource:
 Biology
Biology
Malaria is a life-threatening disease caused by the Plasmodium parasite, which is spread to humans through the bite of an infected female Anopheles mosquito.
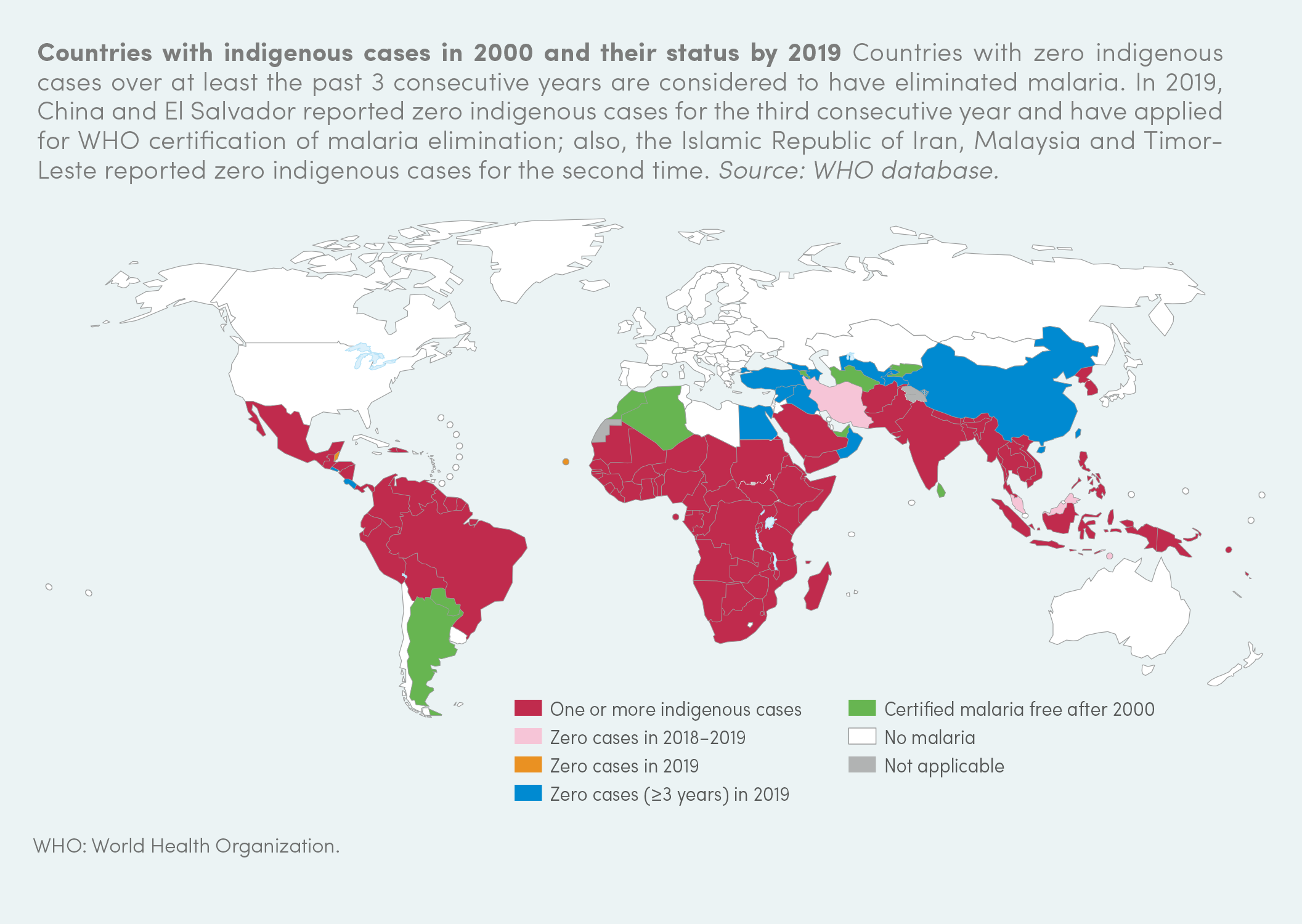
The World Health Organisation (WHO) estimated 229 million cases of malaria in 2019, and 409 000 malaria deaths. Those most vulnerable to malaria are pregnant women and children under the age of five. In 2019, two thirds of malaria deaths worldwide were infant deaths.
Sub-Saharan Africa has the highest number of malaria cases and deaths, but the disease is also widespread in South-East Asia, the Eastern Mediterranean region, the Western Pacific region, and Central and South America.
In the past, malaria was also common in Europe, but the disease was eliminated in 1975 after improvement of socio-economic conditions, agricultural methods, and access to healthcare. Currently there are concerns that climate change will encourage re-introduction or increased transmission of the parasite in tropical and temperate countries.
Malaria is a tropical disease caused by the protozoan parasite Plasmodium. There are five species of Plasmodium that cause malaria in humans, out of which Plasmodium falciparum is the deadliest. Female Anopheles mosquitoes are the carrier (vector) for malaria, transmitting the parasite to humans through bites.
The symptoms of malaria appear about 10 to 15 days after the bite of an infected mosquito. These symptoms include chills, fever, headaches, nausea, vomiting, muscle aches, diarrhoea, and abdominal cramps. Malaria infections also cause anaemia, enlargement of the spleen, and general weakness. Severe forms of the disease lead to convulsions, coma, and often death.
The malaria parasite has a complex life cycle and requires development inside a mosquito and a human host. Mosquitoes carry infectious parasites in their salivary gland. When they bite a person to feed on their blood, they will inject thousands of sporozoites into their bloodstream. These then invade the liver where they mature and multiply into thousands of merozoites, which will invade host red blood cells.
The parasites reproduce asexually inside the red blood cells, which eventually burst to release parasites into the bloodstream to infect new red blood cells. After infecting the red blood cell, parasites completely modify and restructure it, which leads to the development of malaria symptoms. Plasmodium-infected red blood cells become stickier, so they can clump together and stick to the walls of blood vessels, preventing blood flow to vital organs like the brain.
A proportion of parasites develop into gametocytes, which are taken up by mosquitoes as they feed on infected human blood. Inside the mosquito gut, the parasite will sexually reproduce and give rise to more parasites ready to infect a new person through a mosquito bite.
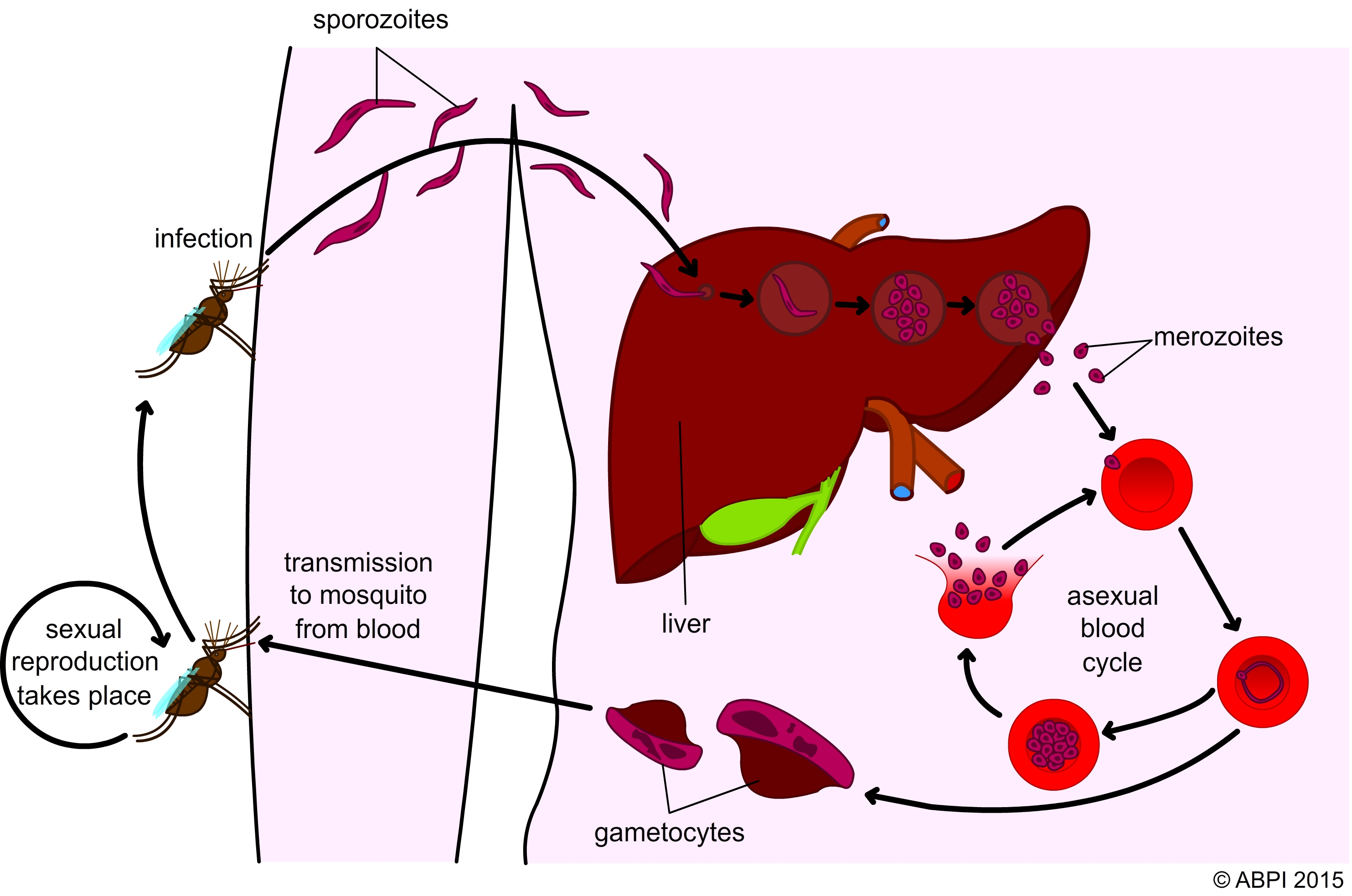
The malaria parasite life cycle
The WHO-recommended treatment for malaria is currently artemisinin-based combination therapy (ACT), as it is the most effective antimalarial therapy. Artemisinin was first isolated in 1972 from the Artemisia annua sweet wormwood plant, but the plant had already been used as a treatment for fever in Chinese herbal medicine for over 2000 years.
In time, Plasmodium parasites can develop resistance to antimalarial drugs. This has been the case for previous treatments like chloroquine and mefloquine. Emerging resistance to ACT is now a major problem in South-East Asia, especially in the Greater Mekong region.

Travellers who go to areas where malaria is a problem are advised to take antimalarial medicines like chloroquine, which suppress the parasite blood stage. This helps prevent the development of symptoms. Treatment starts weeks before the trip and continues for several weeks after leaving the malaria endemic area.
Preventing mosquito bites is another good way to reduce the risk of infection. Insecticide-treated mosquito nets and indoor insecticide spraying are commonly used in countries with high rates of malaria.
Mosquitoes usually feed during the night, so most bites occur while people are asleep. Sleeping under mosquito nets treated with insecticide creates a barrier between humans and mosquitoes, providing a good level of protection against infection. Despite their effectiveness, not all populations at risk can afford them, especially in the poorer endemic areas. Many charities are working hard to increase the numbers of insecticide-treated mosquito nets available in some of the areas of the world most affected by malaria.
Insecticide-treated mosquito nets, such as that shown in the photo opposite, can help reduce deaths from malaria.
Historically, vaccines have played a key role in controlling and eradicating diseases. For decades researchers have been trying to develop a malaria vaccine, but there are several factors that complicate this search. As you have seen above, the Plasmodium parasite has a very complicated life cycle, and it also uses complex mechanisms for evading the immune response of the host.
Several antimalarial vaccines that target different life stages of the parasite are being tested in clinical trials, and the results are encouraging. But control and eradication of malaria will likely be achieved through a combination of antimalarial drugs, a vaccine, and insecticide-treated mosquito nets.