This topic takes on average 120 minutes to read.
 Biology
Biology
 Science
Science
Climate change is making some communicable diseases more common, especially in poorer countries. For example, cholera is a communicable disease which is commonly spread through drinking water which is contaminated with the faeces of an infected person, or by eating seafood or vegetables which have been washed in contaminated water.
Climate change has led to an increase in the incidence of cholera, and this is for a few reasons. Firstly, the increased water temperatures provide ideal conditions for the growth and survival of cholera, making water contamination more likely. Altered rainfall patterns have an impact too, with both extreme heavy rain and droughts being responsible. Heavy rain can cause flooding which means that sewage contaminates water sources, but droughts lead to water scarcity which increases the need to be dependent on contaminated water sources to drink.
Malaria, zika and dengue infections are also on the rise due to climate change. These are all vector-borne diseases, meaning that they are transmitted by a vector organism (in this case, mosquitos). This is because changing climates mean that the vectors (mosquitos) can survive in areas where they couldn’t previously, making the geographical range with the possibility of infection larger. The warmer temperatures can also increase the reproduction of mosquitos by altering their life cycle, increasing the number of vectors. This means that the possibility of infection is higher.
Since the discovery of antibiotics many bacteria have now become resistant. This is known as antimicrobial resistance (AMR).
For example, methicillin resistant Staphylococcus aureus (MRSA) is resistant to several antibiotics, and this can make it difficult to manage this infection in hospitals.
Bacteria become resistant through random genetic mutations which provide an individual organism with an advantageous trait. The advantageous trait prevents them from being killed or inhibited by antimicrobials, and so the organism survives and reproduces. They can then pass this trait on to their offspring, and soon the population without the trait die out and the whole species changes through the process of evolution and natural selection.
Inappropriate prescribing and the misuse of antibiotics are the most common reasons for AMR, and so it is important that patients follow their doctor’s instructions and take their whole course of antibiotics.
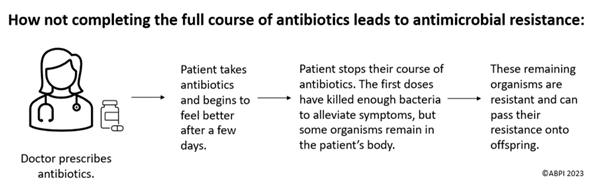
Doctors should also only prescribe antibiotics to patients with bacterial infections, and ensure that the right antibiotic is prescribed for the right infection – remember, antibiotics do not treat viral infections and every antibiotic will kill a different type of bacteria.
You can read more about how bacteria develop AMR on the antimicrobial resistance resource.
Though AMR is mostly caused by the overuse and misuse of antibiotics, scientists have identified that climate change can also cause it.
Scientists have shown that increased air pollution can make antibiotics stop working for some infections, meaning that researchers need to find new antibiotics instead. However, the production of new antibiotics can lead to more air pollution, making this a self-perpetuating cycle.
When leading compounds (which could be new antibiotics) are discovered in vitro, they then need to go through clinical trials to ensure safety and efficacy. If the clinical trial is unsuccessful, then the drug cannot be used and this generates a lot of waste.
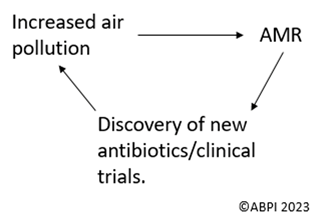
To overcome this, scientists and pharmaceutical companies are now working towards drug repurposing for antimicrobial discovery. For example, drugs that have failed clinical trials for another purpose or that are used to manage another condition can be tested against microbes to see if they work, which reduces emissions from new research and development. An example of this is Auranofin – a drug which is commonly prescribed to treat an inflammatory condition called rheumatoid arthritis. This has been found to be an effective antimicrobial against MRSA and Myocobaterium tuberculosis in vitro, and is now going through clinical trials for antimicrobial use. Researchers hope that, by repurposing drugs, new antimicrobials can be discovered with a reduced research and development process, which will prevent further environmental harm.
To help manage the spread of communicable diseases in plants, farmers can use pesticides, biological control and GM crops. These control methods all impact the environment though.
For example, pesticides can harm animals in the food chain as plants (producers) are at the bottom of the food chain. Therefore, when a plant is eaten by a consumer, that consumer also ingests the pesticide that has been sprayed on the plant. The level of pesticide builds up throughout the food chain in a process known as bioaccumulation, and this can cause the death of organisms which are higher up the food chain. Pesticides may also lead to poor soil quality and reduce the number of pollinators, and all these factors can reduce biodiversity.